When we left Boston, we had several appointments the last few days we were there. Initially, Nicholas had a chest xray and an EKG. After all the tests were analyzed, Dr. Marx found that Nicholas had developed "pleural effusion", or water on the lungs on his left lobe. Because of this, Nicholas's Lasix dosage was tripled in an attempt to get the residual fluid out of his body. We had to go back two days later to check again with another chest xray and a blood draw. The fluid was still there so Nicholas's Lasix dosage was to stay pretty high. Nicholas had to have his blood chemistry checked that day, too, because when a person takes Lasix at a high dosage for a long time, it can mess up the electrolyte levels in the bloodstream, which can lead to cardiac arrhythmia's. Fortunately, Nicholas's blood panel looked good but our goal is (still) to decrease the Lasix to a point that he can stop taking it.
When we left Boston, we had several appointments the last few days we were there. Initially, Nicholas had a chest xray and an EKG. After all the tests were analyzed, Dr. Marx found that Nicholas had developed "pleural effusion", or water on the lungs on his left lobe. Because of this, Nicholas's Lasix dosage was tripled in an attempt to get the residual fluid out of his body. We had to go back two days later to check again with another chest xray and a blood draw. The fluid was still there so Nicholas's Lasix dosage was to stay pretty high. Nicholas had to have his blood chemistry checked that day, too, because when a person takes Lasix at a high dosage for a long time, it can mess up the electrolyte levels in the bloodstream, which can lead to cardiac arrhythmia's. Fortunately, Nicholas's blood panel looked good but our goal is (still) to decrease the Lasix to a point that he can stop taking it.
Another thing that we determined in Boston at the end evaluation was that they would consider Nicholas to have borderline Long QT syndrome. Since I had sent them as much information prior to surgery as possible, they were able to compare his heart rhythm for several years before surgery, immediately after surgery, and the weeks after surgery while we were in Boston. Dr. Marx said that he thinks Nicholas might not have true Long QT, but that because of all the years of surgeries on his heart it might have caused his rhythm to perform differently than if he hadn't had all the surgeries. He recommended that six months to a year from now, we have Nicholas tested with a Holter monitor and exercise stress test to determine for sure if he has Long QT or not. Long QT syndrome is often-times the reason kids will die of sudden cardiac arrest during PE or while playing sports. In a true case of Long QT syndrome, a person's heart rhythm would lengthen, rather than shorten, during exercise. Obviously this is an important piece of information to be aware of, but we cannot really test for sure until Nicholas is all healed up. There are also certain drugs that are routinely prescribed for things like acid reflux and antibiotics for infections that are known to lengthen a person's QT and because Nicholas already has a "borderline long QT", Dr. Marx said he should avoid those certain medications for his lifetime.
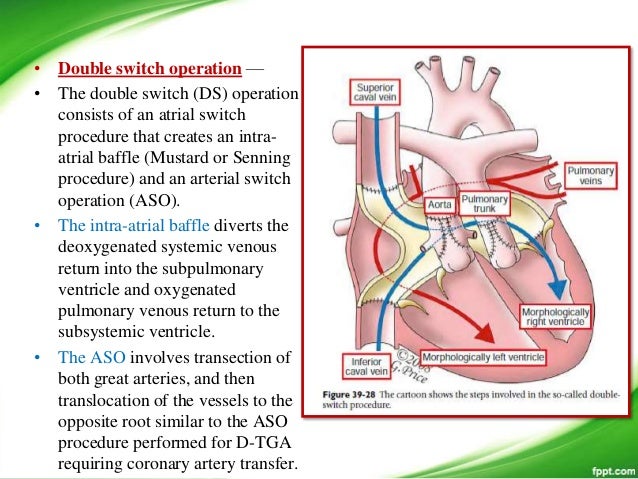
Nicholas has seen Dr. Wright here in Sacramento once already, and we go again this week. He had us take another chest xray before coming in and sure enough, the pleural effusion is still there on the left lung. We will go in for another xray and check up later this week. The really good news is that Dr. Wright said that Nicholas's heart function looks almost normal and that his Left Ventricle is performing like a normal LV. Dr. Wright was almost in tears seeing our boy after all these years of PA bandings and the heartache that came with those 4 attempts at getting Nicholas ready for the Double Switch. He said he couldn't be more pleased at the outcome and that he is so happy that everything has turned out as well as it is so far.
Our heart warrior is getting stronger every day, and is looking more and more like himself. Nicholas is still healing, but daily activities are becoming easier to accomplish and he's closer to his old self every new morning. I am so grateful that he is eating well and looking so good. He has asked me a few times if he will be able to run as fast as the other kids as soon as he's healed, and I have told him that the only way to find out is to go for it!
CHD doesn't go away once the surgery is complete, but I am hoping for a very long lull in heart issues for my boy. After he is done healing from the Double Switch, he will only need to see the cardiologist every 6-12 months for check ups. What a blessing this amazing and quick recovery has been! I am praying that the fluid in his lung goes away and he will be all healed up very soon.
 Lastly, I want to thank anyone who is reading this who has been following Nicholas's story and praying for him and our family. We are so fortunate to have the best families, friends, co-workers, and community. Knowing that there are so many people who love and care about us is a very powerful thing. I hope that I have the opportunity to give back some of what has been given and shown to us these past few weeks and months. Thank you. I am forever grateful.
Lastly, I want to thank anyone who is reading this who has been following Nicholas's story and praying for him and our family. We are so fortunate to have the best families, friends, co-workers, and community. Knowing that there are so many people who love and care about us is a very powerful thing. I hope that I have the opportunity to give back some of what has been given and shown to us these past few weeks and months. Thank you. I am forever grateful.