We got to the hospital at 10:00 this morning. We went straight to the 3rd floor, which is the surgical floor, and they got right to it. We changed Nicholas into his gown and they gave him premed to help him relax. He was quite emotional at the start of it all, but by the time they wheeled him out of the prep area, he was "fine", relatively speaking.
The family waiting area is quite large, and we had plenty of space to get comfortable for the long haul. The surgical assistant, Dr. Kwan, came and talked to us and explained that the operative preparation will take about 1-1.5 hours. This is when they will place all the lines in his arteries to monitor him during the surgery, place the incision and get through all the scar tissue from his previous surgeries, cool his body temperature, start the IV's, etc.
Dr. del Nido said that he expected the surgery portion to last about 5 hours. Nicholas was on bypass for that entire time. He said that the first part of the Double Switch is to do the atrial switch. This means that he re-routes the INCOMING blood from the veins to the opposite atria. He does this by using "native tissue" from Nicholas's pericardium, the tissue that surrounds the heart, and creates a "baffle" - which is like a tunnel - that takes the blood to the opposite side of the upper chambers of the heart.
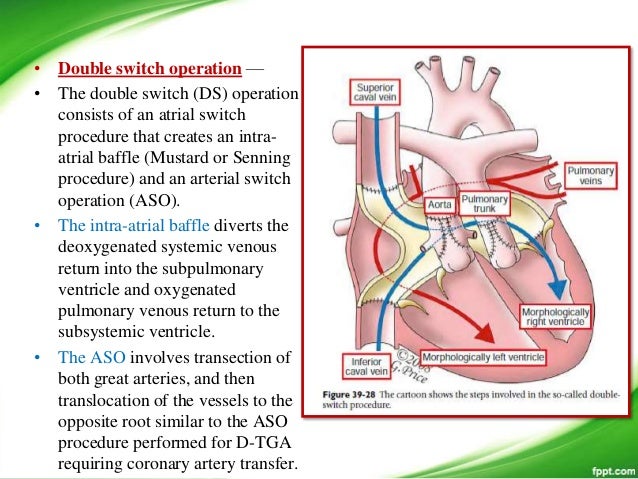 After that is complete, he starts the arterial switch. This is the part where the aorta and the pulmonary artery are switched to the opposite ventricle. He was able to switch the two arteries without any real issues, but when they "started" his heart again, the left ventricle struggled more than he would have liked to see it struggle. He said we kind of expected that to happen to some degree because of the super high pressure the left ventricle was pumping to get blood out through the PA band, and now that the PA band is no longer there, it kind of lost some of the oomph it had been used to pumping against. Also, the right ventricle had been pumping at a systemic pressure beside the left ventricle (causing a "stiff" septum, the wall between the lower chambers) and once the pulmonary artery was attached to the RV, the pressure automatically went down to a normal pulmonary pressure so the septum remodeled and the LV has encroached into the right ventriclular space.
After that is complete, he starts the arterial switch. This is the part where the aorta and the pulmonary artery are switched to the opposite ventricle. He was able to switch the two arteries without any real issues, but when they "started" his heart again, the left ventricle struggled more than he would have liked to see it struggle. He said we kind of expected that to happen to some degree because of the super high pressure the left ventricle was pumping to get blood out through the PA band, and now that the PA band is no longer there, it kind of lost some of the oomph it had been used to pumping against. Also, the right ventricle had been pumping at a systemic pressure beside the left ventricle (causing a "stiff" septum, the wall between the lower chambers) and once the pulmonary artery was attached to the RV, the pressure automatically went down to a normal pulmonary pressure so the septum remodeled and the LV has encroached into the right ventriclular space. Dr. del Nido said that he saw some distortion of Nicholas's aortic tissue above the aortic valve, and that he would fix that part of the vessel as well when he did the switch. He said that he feels like the technical part of the surgery was very successful, and the first 48 hours will tell if the LV will be able to do it's job. Because of all of this, they are "supporting" his left ventricle with quite a few meds and keeping Nicholas paralyzed and heavily sedated. They don't want his heart to do anything but get used to the new job that's been asked of it. They are planning on keeping him like this for the next two days or so.
 It is really hard to walk in and see your big boy on a bed surrounded by wires, tubes, monitors, and laying on a cold pack as big as he is. His body was cold to the touch and they said the heart beats better when it doesn't have to keep the extremities warm.
It is really hard to walk in and see your big boy on a bed surrounded by wires, tubes, monitors, and laying on a cold pack as big as he is. His body was cold to the touch and they said the heart beats better when it doesn't have to keep the extremities warm. Pray for our boy, that his heart does the job it has been asked to do, and that he does not have any unnecessary traumatic setbacks along the way. We decided to come back to the apartment because I don't think I would be able to sleep with all the commotion with them caring for our boy. That was really hard, to leave him. I pray that everything goes smoothly tonight until we get there in the morning. And I hope that he is truly sedated and does not know I left him.

No comments:
Post a Comment